Pheochromocytoma Associated with Renal Agenesis:A Case Report and Review of Literature- Juniper Publishers
Journal of Surgery- JuniperPublishers
Pheochromocytomas are neuroendocrine tumors developed at the expense of cells derived from the neural crest. They occur sporadically in 50-55% of cases, but they can be familial in 5 to 10% of cases and then be isolated or integrated into an inherited syndrome of multiple neuroendocrinopathy. The properly operated pheochromocytoma is radically and definitively cured as long as it is benign and sporadic. Renal anomalies have been reported rarely in this disease. Here we report a rare case of pheochromocytoma associated with renal agenesis. Patient was a female presented with headache and hypertension. In radiologic examinations, an adrenal mass was detected in the right side, with no renal tissue on that side. It was reported an adrenal pheochromocytoma in histopathology. Renal agenesis confirmed during surgery. All of the patient’s symptoms alleviated after the resection of tumor. Considering association of renal abnormalities with pheochromocytoma, it is recommended to perform genetic analysis and kidney evaluation in cases with MEN type 2 or each of its components.
Keywords:Pheochromocytoma; Renal agenesis; RET gene mutation
Introduction
Pheochromocytoma and unilateral renal agenesis/hypoplasia are well-reported conditions. Their combination, however, is rare with few cases reported [1-3]. Rearranged in Transfection (RET) gene mutations are proven to cause both of these conditions. RET mutation as a possible common mechanism of the both conditions is discussed briefly along with literature review and possible clinical implications of the association.
This coexistence of paraganglioma / pheochromocytoma and renal agenesis may have a common genetic mechanism in the form of Rearranged in Transfection (RET) gene mutation. This is a well-characterized gene, mutations of which are known to be associated with both conditions. Current knowledge of the role of RET gene in both conditions is reviewed to put forth RET mutation as the possible common underlying genetic mechanism along with possible clinical implications of the combination.
Observation
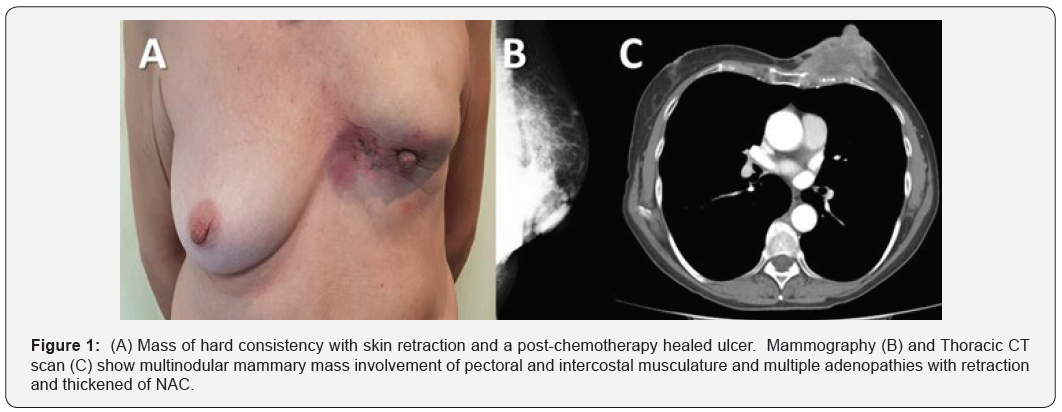
Pheochromocytoma and renal agenesis are commonly reported conditions. Their coexistence, however, is rare, with few cases reported. The case of 31-year-old female was admitted for headache and occasional night sweating. Family history was negative for any significant disease. Physical examination was normal except for hypertension (BP= 160/90). Laboratory examinations consisted of complete blood count (CBC), serum and urine biochemistry, serum renin and aldosterone level were all-normal. Abdominal MRI and abdominal CT scan detected in the right side an adrenal gland (60-80-40 mm ) with calcifications and necrosis area driving back the liver and the vena cava right renal agenesis. Therefore, urine VMA and NMN checked which both were higher than normal. MIBG scan showed increased radiotracer uptake in adrenal mass (Figure 1).
Surgery
Right adrenalectomy
Steps of surgery:
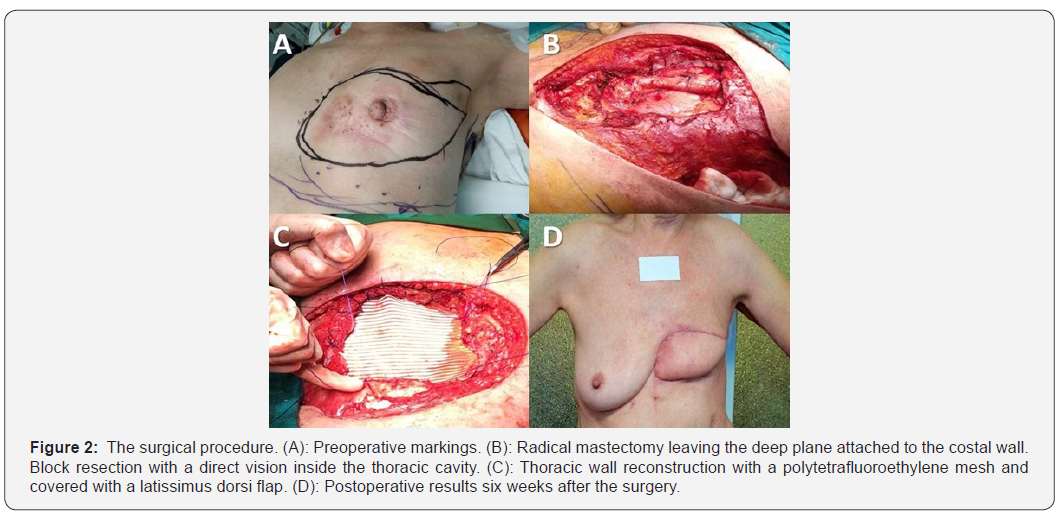
a) Laparotomy (Figure 2).
b) Installation: The patient is installed in an intermediate position between the dorsal and lateral decubitus.
Procedure: Vascular access, from the inferior vena cava (Figures 3 and 4).
Resection of the tumor mass (Figure 5).
Follow up: Favorable and patient discharge 6 days later.
Anatomopathological study: In favor of a pheochromocytoma (Figure 5).



On follow-up, patient is normotensive and asymptomatic.
Discussion
This coexistence of paraganglioma / pheochromocytoma and renal agenesis may have a common genetic mechanism in the form of Rearranged in Transfection (RET) gene mutation. This is a well-characterized gene, mutations of which are known to be associated with both conditions. Current knowledge of the role of RET gene in both conditions is reviewed to put forth RET mutation as the possible common underlying genetic mechanism along with possible clinical implications of the combination. With a mutated common gene, it is logical to expect association of congenital renal abnormalities and chromaffin tumors (those due to RET mutations). However, we noted one case of renal agenesis associated with chromaffin tumors in literature [1-4]. To our best knowledge, we are reporting a case of pheochromocytoma associated with renal agenesis. The following discussion is an endeavor to explain this association in the light of role of RET gene uncovered in embryology and cancer biology.
Rearranged in Transfection gene is located on chromosome 10 and gene product is a cell membrane receptor of tyrosine kinase family. Ligand (molecule which attaches to receptor) of glial cell line-derived neurotrophic factor (GDNF) family binds to RET receptor resulting in activation of multiple downstream pathways that promote cellular proliferation, survival and/or differentiation. Gain of function mutations cause persistently activated receptor in the absence of ligand promoting malignant transformation. RET mutations are well-established cause of multiple endocrine neoplasia type 2 (MEN2) syndromes (medullary carcinoma thyroid, adrenal pheochromocytoma, ganglioneuromas) [5,6]. Incidence of RET mutation in paraganglioma is variably reported but estimated to be 5% in a recent review article [5,7].
How can loss of function phenotype (renal agenesis) possibly coexist with a gain of function phenotype (pheochromocytoma)? Different RET mutations in different cases are described [2,8]. A subset of RET mutation (called Janus mutation) may have a negative role in neural and/or renal development but promote cellular proliferation. Experimental evidence for such mutation was found when a particular type of RET mutation was found to promote cellular proliferation but which impaired GDNF action on RET on cellular migration and differentiation in vitro [9] about our case of renal agenesis with pheochromocytoma described previously [2]. Further, same gene mutation may manifest with only loss of function phenotype in one generation but with loss and gain of function mutation in a different generation, for example, familial renal agenesis with medullary carcinoma thyroid in a mother and with Hirschsprung disease in son [8]. Similarly, “carriers” of MEN2 patients having renal agenesis have been described, who possibly show only one manifestation of the full spectrum of RET mutation effects [10]. Precise molecular mechanisms in such cases remain to be to be elucidated completely
However, we do realize potential problems in conjuncture of RET mutation being an underlying common link for renal agenesis and paraganglioma. It is well known that unilateral renal agenesis is a common condition (1 in 1000 live births) and so association with paraganglioma may be incidental. Also, reported RET mutation incidence in renal agenesis is variable, quoted as 7–20% in stillborn fetuses [7,11]. However, this may explain as a common final pathway of RET gene being influenced by mutation in other modulating genes. It can also be due to low penetration of RET gene to cause renal agenesis as compared to high penetration for malignant transformation [10]. In our case, we could not carry out testing for RET gene due to financial constraints of the patient.
Conclusion
There are a few reports of renal abnormalities in patients with pheochromocytoma. Genetically, the significance of RET protooncogene gene and its encoding protein related to tyrosin kinase family has been documented in the induction of metanephric blastema and ureteric bud during kidney morphogenesis . Mutation of this gene is known to be responsible for developing MEN type 2A, renal agenesis or severe dysplasia. The association of renal abnormalities with pheochromocytoma, it is recommended to perform genetic analysis and kidney evaluation in cases with MEN type 2 or each of its components.


Comments
Post a Comment