Paramedic Student Progress in Medication Calculation- Juniper publishers
Journal of Surgery- JuniperPublishers
Emergency Medical Service (EMS) is one of the health professions that society requires. EMS involves the use of certain emergency medications to save lives. Therefore, EMS providers (paramedic) should acquire sufficient training in medication administration. A part of the training focuses on the knowledge of medications, indications for use, contraindications (side effects), and dosing skills considering the type of disease, concentration of medication, age, or weight of the patient. A student who is trained to be a paramedic should be adequately skilled to properly calculate the dosage of medications. This study aims to determine the paramedic students’ ability and its progress in medication calculation while studying in EMS program in Prince Sultan Bin Abdulaziz College for EMS (PSCEMS), King Saud University (KSU), Riyadh, Saudi Arabia.
Literature Review
A few research articles were found concerned with medication calculation abilities among paramedic students. Two cross-sectional studies by Kathryn et al. [1,2] were conducted using descriptive paper-based questionnaire administered to undergraduate paramedic students to assess their basic mathematical and medication calculation performance. Student attitudes regarding their medication calculation performance and answers to a series of basic mathematical and medication calculation questions were collected. The study found that the mean score of the correct answers was 39.5% with only 3.3% of students (n=3) scoring greater than 90%, and 63% (n=58) scoring 50% or less. Conceptual errors were 48.5%, arithmetical 31.1%, and computational 17.4%. The two studies concluded that undergraduate paramedics have fundamental deficiencies in performing accurate calculations with conceptual errors indicating the lack of mathematical understanding [1,2].
Another report of a cross‐sectional study that was conducted by Mcmullan et al. [3] in 2006 in United Kingdom using a medication calculation test given to 229 second year nursing students and 44 Registered Nurses (RN) attending a non‐medical prescribed program. It reported no significant statistical difference between nursing students and RNs in their overall medication calculation skills. It, however, suggested a more statistically significant superiority of RNs over the students to perform basic numerical calculations and calculations for solids, oral liquids, and injections. Therefore, 55% of students and 45% of registered nurses failed the numeracy test, while 92% of students and 89% of nurses failed the drug calculation test [3]. Bernius et al. [4] conducted a questionnaire requiring calculations of medication doses and volumes of two groups and compared the rate and extent of errors. Of the 523 advanced life support prehospital care providers questioned, 246 answered questions using the pediatric code card and 277 answered questions without using the card. The mean of individual percentages of correct responses were 94% for the group aided with the code card and 65% for the group unaided with the card (percentage difference, 29%; 95% confidence interval [CI], 25-31%; p < 0.001) [4].
LeBlanc et al. [5] compared the assessment performances of paramedics in calculating medication dosages in low-stress and high-stress conditions. Thirty paramedics were asked to calculate medication dosages in a quiet classroom (low-stress) and immediately after working (high-stress). The results suggested that the types of stressors encountered in clinical situations can increase medical errors, even with highly experienced individuals. The paramedics obtained lower accuracy scores in the high-stress condition than in the low-stress condition (43% (95% confidence interval [CI]: 36.9-49.2) vs. 58% (95% CI: 48.6-67.1), p < 0.01 based on univariate analysis) [5].
Another cross-sectional study by Malcolm et al. [6] utilized a medication calculation questionnaire in an intensive care paramedic course with twenty paramedics. The questionnaire consisted of medication (seven questions) and mathematical (five questions) calculations. Four (20%) students answered all 12 questions correct and five (41.6%) acquired 50% or less. The average score was 8.6 (71.7%) correct, SD 2.8 correct, range 3 to 12 correct questions. There were 8 (40%) conceptual errors, 12 (60%) arithmetical errors, and 5 (25%) computational errors. The results highlighted the paramedics’ mathematical skills at a potential risk to patient safety and suggested regular continuing mathematical and medication calculation practice and education [6]. Eastwood et al. [7] conducted a cross-sectional study using a questionnaire containing medication calculation and arithmetic questions with the students before, during, and at the end of semester for firstyear undergraduate paramedic students. The students initially demonstrated a poor ability to complete mathematical and medication calculations without the assistance of computational devices. An intervention of an appropriate education and practice led to a significant improvement. Medication calculation and mathematical ability were markedly improved following the tutorials; the mean score of correct answers were 1.74 (SD 1.4) before and 4.14 (SD 0.93) after (p<0001). When comparing the correct results for the same question type, four of five different medication calculations illustrated statistically significant differences: volume of medication drawn up 10 v 57 p<0.0001, infusion rate 29 v 31 p=0.717, drip rate 16 v 54 p<0.0001, volume from a syringe 30 v 59 p<0.0001, and dose 42 v 62 p<0.0001. Total errors reduced significantly from 188 to 45 [7].
Nonetheless, a prehospital-related electronic database review by Kathryn et al. [8] using the Ovid and EMBASE systems in Monash University Library located 59 relevant articles from 1,154 articles, in which only 3 met the review inclusion criteria. The review revealed significant deficiencies in mathematical proficiency among the paramedics sampled and questioned if undergraduate paramedic students are capable of performing the required drug calculations in a non-clinical setting [8].
Method
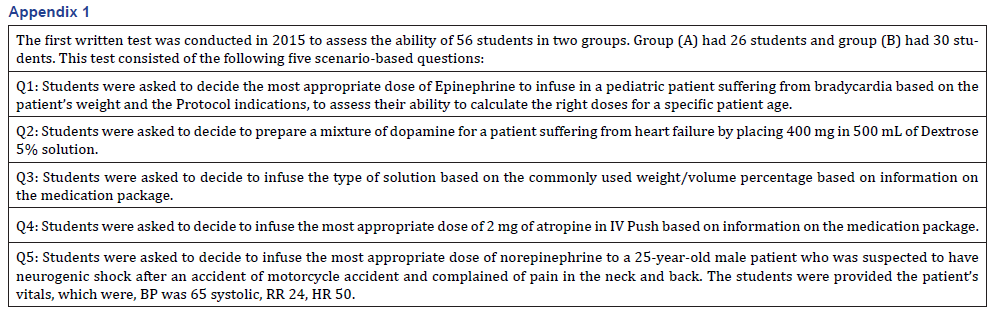
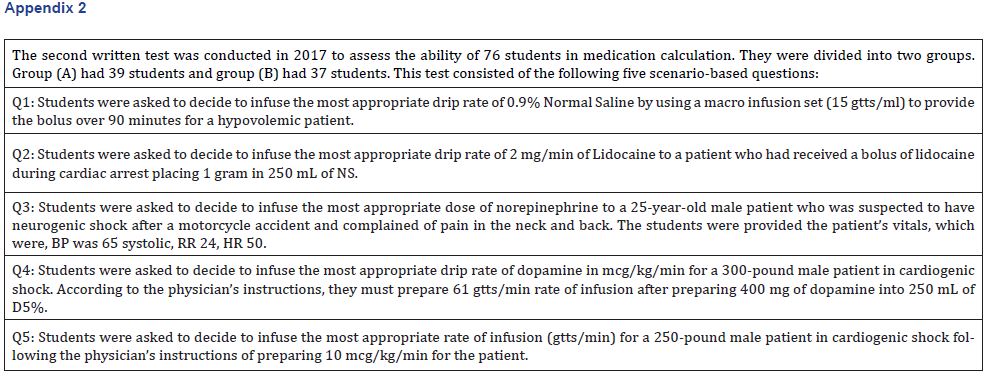
This longitudinal and post-interventional study aimed to determine the ability of EMS students in medication calculation during the 3-year EMS program. End of the semester tests were conducted twice on 15 June 2015 and 27 May 2017 at PSCEMS. The interventions applied were a 3-credit hour Emergency Medications course (EMS 224) offered in the 4th semester (2015) and a 5-credit hour Critical and Intensive Care Practice course (EMS 421) offered in the 8th semester (2017). Therefore, the inclusion criterion in both tests was the enrollment in the two courses. Participants were all male students and distributed into two groups for each course according to an automated academic registration system. Nevertheless, the same instructor taught in both groups for each course. Each test consisted of 5 questions. They were designed based on the learning outcomes for each course. Moreover, the questions focused on the students’ ability to calculate and decide on the dose or rate of infusion for certain scenarios. The students were allowed to use calculators in both the tests. Only one question from the first was repeated in the second tests. The first written test for the course (EMS 224) was conducted on 15 June 2015, with 56 students divided into 2 Groups. Group (A) had 26 students and Group (B) had 30 students. This test consisted of 5 scenario-based questions, as shown in Appendix 1. EMS 224 course aimed to “discuss principles of pharmacology, pharmacokinetics, pharmacology classifications, and pharmacodynamics.” One of its intended learning outcomes was to “prepare students to calculate the medication doses, medication volume, and infusion rate of pharmacological agents in a given situation.”. The second written test was conducted on 27 May 2017 at PSCEMS, with 76 students divided into 2 groups. Group (A) had 39 students and group (B) had 37 students. This test consisted of 5 scenario-based questions, as shown in Appendix 2. The course aimed to “introduce students to the fundamentals of intensive and critical care transport.” One of its intended learning outcomes was to “demonstrate knowledge of specific medications common to patients requiring critical care transport.” Data were manipulated and analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.0 software including Analysis of Variance (ANOVA).
Result
A 5-question test was conducted twice, at the end of the 4th semester on 15 June 2015 and 8th semester on 27 May 2017 during the 3-year EMS program. In general, the tests aimed to determine the ability of students to calculate medication doses, volume, and infusion rate of pharmacological agents in a given situation.
The following is the performance of the groups with respect to the individual questions:
As illustrated in Table 1 the outcomes of the EMS 224 students’ performance of Group (A) (n=26) are as follows: The first question, Q1, focused at determining the infusion dose of Epinephrine for a pediatric patient with bradycardia, and 20 students (76.9%) answered it correctly. The second question, Q2, was related to preparing a mixture of Dopamine for a heart failure patient by placing 400 mg in 500 mL of Dextrose 5% solution, and 23 students (88.5%) answered it correctly. The third question, Q3, involved the infusion of a solution according to information on the medication label of 10% (100 mg/ml) Calcium Chloride injection. Eighteen students (69.2%) answered Q3 correctly. The fourth question, Q4, pertained to an infusion of a dose of 2 mg of (400 mcg/ml) atropine in IV Push as shown on the medication label, and 16 students (61.5%) answered correctly. The last question, Q5, involved the infusion of a dose of norepinephrine to a 25-yearold male patient suspected to have neurogenic shock following a motorcycle accident, and 23 students (88.5%) answered the question correctly. Tables 3 and 4 illustrate that the mean count and std. divination of the scores of groups (A) were 20 and 3.082. The tables show that the highest and lowest number of students who answered the questions correctly ranged from 23 to 16, with a variance of 9.500.
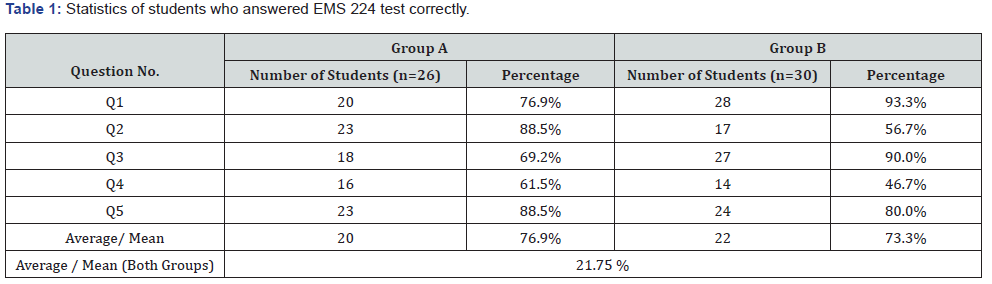
As illustrated in Table 1 the following are the results of the same test (EMS 224) by group (B) (n=30): Out of 30 students, 28 (93%) answered Q1 correctly, 17 (56.7%) answered Q2 correctly, 27 (90%) answered correctly in Q3, and only 14 (46%) answered Q4 correctly. In Q5, 24 students (80%) gained correct scores. Tables 3 & 4 illustrate that the mean count and std. divination of the scores were 22 and 6.205, respectively. The tables show that the highest and lowest number of students in this group who answered the questions correctly ranged from 28 to 14, with a variance of 38.500. The average combined mean and percentage of groups A and B were 21 and 75.13%, respectively.
As illustrated in Table 2, The outcomes of the EMS 421 students’ performance of Group (A) (n=39) are as follows: The first question, Q1, was regarding the infusion of a drip rate of 0.9% Normal Saline by using a macro infusion set (15gtts/ml) to give the bolus over 90 minutes for a hypovolemic patient. Twenty students (51.3%) answered Q1 correctly. Q2 was to determine an Infusion drip rate of 2mg/min of Lidocaine to a patient who had received a bolus of lidocaine during cardiac arrest placing 1 gram in 250mL of Normal Saline (NS). Twenty-one students (53.8%) answered it correctly. Q3 involved the infusion of a dose of norepinephrine to a 25-year male patient suspected to have neurogenic shock following a motorcycle accident. Only 11 of 39 students answered it correctly, which represent 28.2%. Q4 was related to preparing in mcg/kg/min 61gtts/min rate of infusion after preparing 400 mg of Dopamine into 250 mL of D5% for a 300-pound male patient in cardiogenic shock. Only 13 students (33.3%) scored it correctly. Q5 was related to an infusion of a rate (gtts/min) for a 250-pound male patient in cardiogenic shock and then prepare 10mcg/kg/min for this patient. Only 17 students (43.6%) answered it correctly. Tables 3 and 4 illustrate that the mean count and std. divination of scores of this group (A) were 16.40 and 4.336. The tables show that the highest and lowest number of students in this group who answered the questions correctly ranged from 21 to 11, with a variance of 18.800.
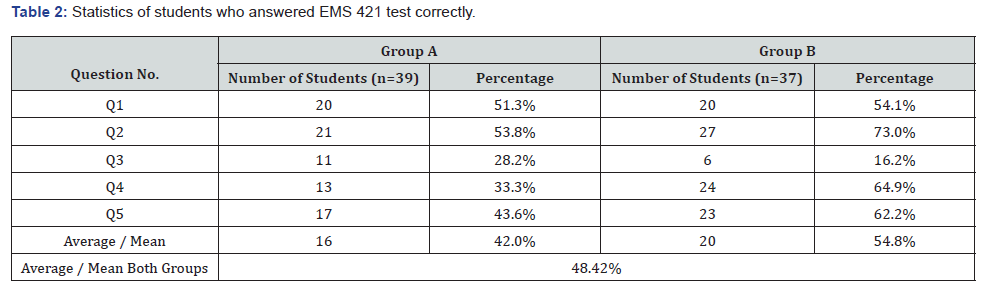
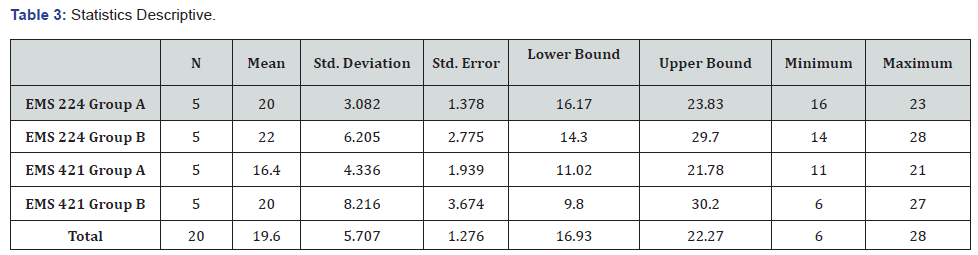
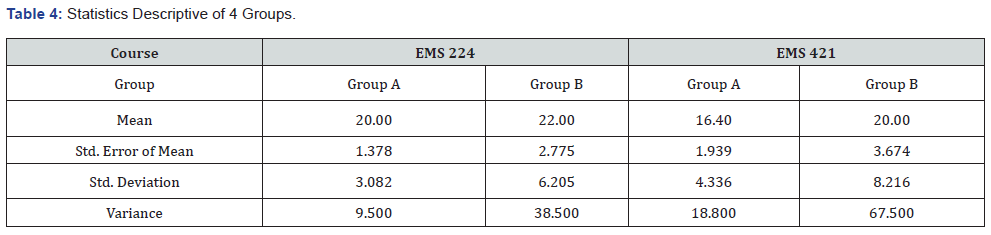
As illustrated in Table 2, The same test (EMS 421) was taken by Group (B) (n=37), in which 20 students (54.1%) answered Q1 correctly, 27 students (73.0%) answered Q2 correctly, only 6 students answered Q3 correctly, which represent (poorly) 16.2%. In Q4, 24 students (64.9%) scored correct answers, whereas in Q5, 23 students (62.2%) answered correctly
Tables 3 & 4 illustrate that the mean count and std. divination of scores were 20 and 8.216. They show that the highest and lowest number of students in this group who answered the questions correctly ranged from 27 to 6, with a variance of 67.500. The average combined means and percentage of groups A and B were 18 and 48.42%, respectively.
Comparison Analysis
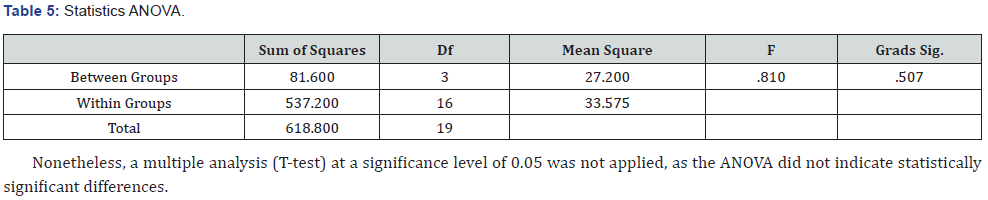
Considering comparison analysis between and within groups in test performances, a multiple comparison, ANOVA was utilized. The p-value > 0.05 indicated no significant differences among students’ performance within the groups, whereas p-value < 0.05 indicated a significant difference. Table 5 illustrates that the value of F is .810 variances between groups than within the groups. The F significance is more than 0.05, indicating no significant statistical differences in the students’ performance regarding the answers of the 5 questions in each group over the years. The mean count of EMS 421 Group A is certainly lower than that of the other groups.
Discussion
This discussion highlights the important characteristics of the experimental results obtained in order to determine the ability of paramedic students and the progress of their ability in medication calculation while studying in EMS program in PSCEMS, KSU, Riyadh, KSA. Two groups of students were investigated in a classroom at two different occasions (course EMS 224 test in 2015 and course EMS 421 test in 2017). Five mathematical questions were used, including calculate doses, medication volume, and infusion rate of pharmacological agents in a given situation. The results showed a fairly satisfying level of performance in the first test when compared with the studies reviewed. The result, however, showed variability in the students’ performance in the 2 tests. As a matter of fact, students scored higher in the first test, as 75.13% of students in 4th semester answered 5 questions correctly whereas in the second test, in which 48.42% of students in 8th semester scored answers correctly.
The first course focused on the basic knowledge of pharmacology, including medication calculation, while the second course emphasized on critical care. The probable reason the students scored higher could be that they had recently completed the pharmacology course. When students took the medication calculation test after a long time, their knowledge and ability seemed to be diminished. One of the questions was repeated in the first and second test. The scores in that specific question indicate that the students performed quite differently in both tests. The number of students who answered it correctly in the first test was 47 out of 56 and 17 out of 76 in the second test. In agreement with Kathryn et al. [1] and Malcolm et al. [6], this study asserts that paramedic students are not sufficiently prepared for medication calculation and that they are in greater need for pharmacology refreshments and skills development courses. On the other hand, this study, in agreement with Malcolm et al. [6] and Eastwood et al. [7], suggested that students could score better in tests after enrolling in an educational intervention, as in the case of the first test of this study. This indicates that the more the students are separated from the educational intervention, the less their ability in medication calculation would become. Moreover, the results of the first test did not correspond with the results of LeBlanc et al. [5] when they tested students in low stress environment, in which our study showed superior results.
The results of the second test correspond with the results of Kathryn et al. [1,2], as it was found that the mean score was 39.5% and 92% of students and 89% of nurses failed the drug calculation and showed lack of medication calculation proficiency. Moreover, in the second test, the groups appeared to have a large number of students with poor performance, which affected and skewed down the total average scores. This raises a concern that the results of the first group might have been affected by the poor scores of the students in the same group. Nonetheless, both of our tests were unaided and conducted in low-stress situations. When compared with Mcmullan et al. [3] and Bernius et al. [4], we found their correct scores to be 65% and 58%, which are close to the results of this study.
Most EMS (Paramedic) programs offer a pharmacology course in the early stage of the program. Subsequently, EMS students get involved in completing the other core courses of the program, namely, Trauma emergencies and medical emergencies. Similarly, the curriculum of PSCEMS does not offer any courses on medication calculation after the first pharmacology course in the 4th semester, leaving the responsibility of enhancing the knowledge and skills on the students themselves. This signifies that students who could not refresh their knowledge and skills might end up at the labor market or face difficulties in any future competency testing. Therefore, an ongoing educational opportunity in medication calculation is suggested for paramedic students to overcome their deficiencies and maintain their competency. Another challenge that requires attention is the competency level. The level of difficulty increases for the students in the later stages of the program. The lower-level questions were asked in the initial phase of course and vice versa. In the stage of critical care, complicated questions were asked. Therefore, the competency level, from the beginner to intermediate to professional advanced, needs to be considered. The fact that the students in our study took the second test in last semester of the program, at a time when students might feel exhausted and less enthusiastic regarding high achievement, could be one of the reasons for such deficiencies in their results. In addition, some students put tremendous efforts to perform well in the tests, with little intention on understanding the applicability in real life practice.
The limitations of this study include the small sample size, non-stressful classroom test, and the varying number of students between two courses, owing to high academic registration of students in the second course. Moreover, the study included students from only one Saudi university, which might limit the generalization of the results.
Conclusion
Paramedic students show some strength in their ability of medication calculation immediately after completing pharmacology course. Their ability, however, diminishes as they proceed in the EMS program. Therefore, an ongoing educational opportunity in medication calculation is suggested for paramedic students to overcome their deficiencies and maintain their competency.
To read more articles in Journal of Surgery
Click on: https://juniperpublishers.com/journals.php


Comments
Post a Comment