Juniper Publishers| Superior Mesenteric Vein Thrombosis as a Complication of Crohn’s Disease: An Unusual Case
Journal of Surgery- JuniperPublishers
Abstract
Background: Mesenteric venous thrombosis (MVT) is a rare but potentially catastrophic clinical complication, which may lead to ischemia or infarction of the intestine.
Methods: We report here a case of superior mesenteric vein (SMV) thrombosis in a 21 year old male patient with no history of Crohn’s disease or other risk factors of thrombosis. Patient was admitted to the hospital with the signs and symptoms of small bowel obstruction. He was taken to the operating room after the initial diagnostic tests and underwent partial small bowel resection followed by end to end anastomosis. İntraoperative diagnosis was acute mesenteric ischemia (AMI).
Results:Final pathological evaluation of the resected specimen was confirmed as demonstrating features of Crohn’s disease.
Conclusion: Crohn’s disease should be considered as one of the underlying causes when AMI is the diagnosis.
Keywords: Crohn’s disease; Acute mesenteric ischemia, Intestinal obstruction
Abbreviations: AMI: Acute mesenteric ischemia; CT: Computed tomography; IV: Intravenous; MVT: Mesenteric venous thrombosis; SMV: Superior mesenteric vein
Introduction
From environment to patient
Acute mesenteric venous ischemia is a serious acute abdominal condition requiring early diagnosis and intervention to improve outcome. Surgical resection is still the main curative approach [1]. Acute mesenteric ischemia (AMI) can be caused by various conditions such as arterial occlusion, venous occlusion, strangulating obstruction, and hypoperfusion associated with nonocclusive vascular disease, and the CT findings vary widely depending on the cause and underlying pathophysiology [2,3]. Superior mesenteric vein (SMV) stenosis as a consequence of mesenteric fibrosis, causing the development of small bowel varices, is an unrecognised association of Crohn’s disease [1,4]. Mesenteric venous thrombosis (MVT) accounts for 5 to 15 percent of all mesenteric ischemic events and usually involves the SMV; the inferior mesenteric vein is involved only rarely. The diagnosis is often delayed, and most cases are identified either at laparotomy or at autopsy. MVT is potentially catastrophic clinical condition which may lead to ischemia or infarction of the intestine [2,5]. Diagnosis of MVT in inflammatory bowel disease is difficult as patients frequently present with nonspecific abdominal discomfort which may delay diagnosis and initiation of treatment [6,7]. We report here a case of SMV thrombosis in a 21 year old male patient with no history of Crohn’s disease or other risk factors of thrombosis.
Case Report
Admission and Physical Exam
A 21-year-old male complaining of abdominal pain predominantly on the right lower quadrant was admitted to our hospital from the emergency department on March 2010. The pain had started on the previous day around the umbilicus, it was dull, non-radiating, not related to meals and was only partially relieved by lying in prone position. On admission, he was vomiting, had minor diarrhea and subclinical fever (37.8°C). Physical exam revealed abdominal tenderness on all quadrants but rigidity. Bowel sounds were absent on admission, he had no ascites or splenomegaly. Rectal exam revealed normal anatomy and loose stool.
Diagnostic and Therapeutic Protocol
Abdominal and chest X-ray series and abdominal ultrasonography, complete blood count, blood chemistry including electrolytes, kidney and liver function tests as well as blood gasses were performed and studied upon admission. Chest X-ray was normal, upright abdominal X-ray demonstrated air-fluid levels revealing small bowel obstruction. Abdominal ultrasound detected minimal intraabdominal fluid in the lower quadrants. Abdominal helical computed tomography (CT) was also performed as an adjunct for differential diagnosis. CT findings were reduced enhancement of the small bowel wall, mural thickening, mesenteric fluid and congestion of small mesenteric veins. Vital signs were measured and recorded as following: Blood pressure; systolic: 100mm/Hg, diastolic: 65mmHg, pulse: 110 beats/min, respiratory rate: 20/min, temperature: 37,8°C. According to the laboratory results, WBC: 13.5x103/ml, Hb: 12,2 g/dL, Hct: 36,8%, RBC: 4,5x106/mm3, PLT: 236x103/mm3, ALT: 51 U/mL, AST: 48 U/mL, GGT: 58 U/L, ALP: 83, Total protein: 6,8 g/dL, Albumin: 3,6 g/dL, Total bilirubin: 0,9 mg/dL, Direct bilirubin: 0,3 mg/dL, Creatinine: 0,91 g/dL, BUN: 34 mg/dL, Na: 139 mEq/L, K: 4,3 mEq/L, Cl: 95 mEq/L Ca: 8,3 mg/dL and arterial blood gas measurements were pH: 7,34, HCO3: 22 mEq/ lt, pCO2:41 mmHg, pO2: 87 mmHg. Hematology workup showed no evidence of congenitally inherent hypercoagulable state.
The patient developed signs of small bowel obstruction that required urgent laparotomy. He was taken to the operating room and upon meticulous abdominal exploration, 90 cm of necrotic small intestine with extreme venous congestion 30 cm proximal to the ileocaecal valve was observed. Creeping fat along the small bowel serosa was also noticed (Figure 1). Necrotic small bowel was resected with clear surgical margins of 1 cm. at both edges and saved for pathology. Operation was completed after constructing an end to end bowel anastomosis and placement of a silicone abdominal drain.
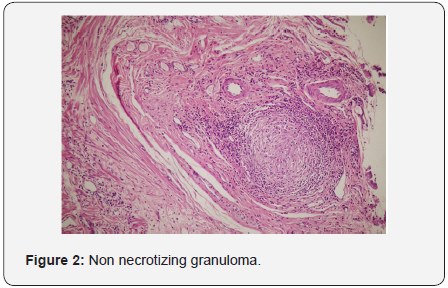
Follow-up
Adequate fluid and electrolyte resuscitation was maintained via IV crystalloid solutions according to the daily output during the postoperative period. On the third postoperative day, IV fluid replacement was tapered and oral fluid intake started. Patient tolerated oral intake and he switched to soft food on the fourth postoperative day and all IV fluids stopped. The silicone abdominal drain was withdrawn and patient was discharged on the fifth day following the operation. Histopathologic examination of the resected specimen showed underlying MVT with evidence of Crohns disease (Figure 2). Further treatment with sulfasalasine and follow-up was managed by the gastroenterology clinic.

Discussion
AMI is a life-threatening condition, with a reported mortality rate of 50-90% that requires early diagnosis and treatment. Signs and symptoms associated with AMI are common to various intra-abdominal pathologic conditions. The severity of abdominal pain is usually out of proportion to the physical findings. Crohn’s disease is a chronic inflammation of the digestive tract and abdominal pain and diarrhea are the most common symptoms of Crohn’s disease [6]. SMV stenosis as a consequence of mesenteric fibrosis, causing the development of small bowel varices, is an unrecognised association of Crohn’s disease [8-10].
Helical CT is a highly sensitive method to rule out intestinal ischemia in the context of acute small-bowel obstruction. There is no radiographic gold standard for the diagnosis of SMV thrombosis, but a CT scan with intravenous and oral contrast, and mesenteric angiography, are the most useful diagnostic modalities. Angiography has been the reference standard imaging examination; however, the role of CT in this setting has expanded with the advent of helical CT scanners [6]. Magnetic resonance angiography holds promise but still remains investigational. It should be noted that, on average, 10% of SMV thrombosis cases will be missed on abdominal CT scan or ultrasound. Attention must be focused on the presence of the signs of strangulation and ischemia: reduced enhancement of the small-bowel wall, mural thickening, mesenteric fluid, congestion of small mesenteric veins, and ascites. A diagnosis of ischemia can be made if enhancement of the bowel wall is reduced or if at least two of the other signs are found.
In the evaluation and initial management of this particular case, CT scan and clinical findings were our most practical guide. Due to the inconvenience of our emergency department, angiography was not available. Until the pathological confirmation, ethiology of this episode of AMI was obscure. As detected in the resected intestinal specimen, erosions and ulcerations, hyperplasia of the muscularis mucosae, irregular intestinal luminal border, mucin depletion, scattered crypt abscesses, branched and budded crypts, fissure formation, nonnecrotizing granulomas, increased inflammatory cells within the lamina propria were all remarkable for Crohn’s disease. In summary, AMI is a challenging clinical problem with various causes for which diagnosis and therapeutic interventions must be prompt. Crohn’s disease should be kept in mind within the ethiology of this frequently fatal condition.

Comments
Post a Comment