Juniper Publishers| Oral Surgery in the Human Microbiota Era the role of Periodontal Bacteria
Journal of Surgery- JuniperPublishers
System biology and Human microbiota
Recent studies have highlighted the oral cavity as a complex biological system organized into several micro and nanoscopic scales, as described by an interdisciplinary field of study using a holistic approach. In this context the recent introduction of the technology of Next Generation Sequencing (NGS) has shed new light on human genomics, but,more especially, has increased the knowledge of the bacterial populations normally resident in the human tissues and called microbiota. NGS, also known as high-throughput sequencing, is a procedure that is able to perform the sequencing in a few hours of both the entire human genome and also the complete profile of the ribosomal gene set or certain genes of interest related to a specific microbiota (metagenomics). Many human tissues, such as the skin, oral cavity, nose, upper air-ways, stomach, lower intestine, and the genito-urinary tract, are colonized by resident populations of bacteria. This complex microbial community performs many essential functions, including a protective effect in preventing opportunistic infections through the competitive exclusion of pathogenic species or by modulating the immune response in the host. In other cases it provides a fundamental contribution to normal functioning in its ecological area (tissue) i.e.in the digestive function in the gastro intestinal tract. The microbiotas in the healthy subjects must be in a strict range of homeostasis with the tissues in which they exist. In fact, the reasons why these bacterial communities could be harmful in humans is that a group of some opportunistic bacteria can infect body areas, normally free from microbial colonization, as a result of normal host defenses being compromised. In particular, in oral microbiota we find a group of anaerobic bacteria that are historically related to periodontal disease, which according to the latest research, are able to invade other body regions or organs from the oral district. The latest evidence shows that these severe infections were most likely a consequence of a bacteremia from oral tissues due to surgical acts or caused in patients after oral hygiene procedures, such as tongue scraping [1].
The vengeance of periodontal bacteria “only for aesthetic effect”
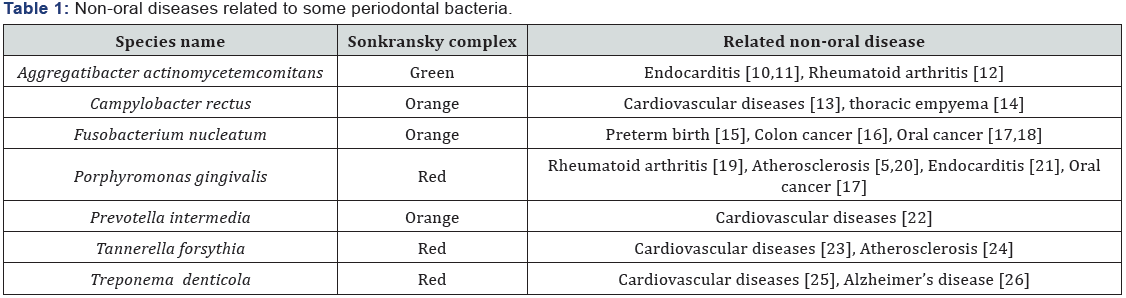
In the 1990s Sigmund Socransky published a fundamental work, in which he used association criteria in healthy and diseased subjects to categorize the bacterial species involved in the initiation and progression of periodontal disease. He divided the several complexes of bacteria into groups and labeled them with colors, the categories were based upon the association with the disease (Table 1). 25 years after this publication some crucial new information has been discovered about these anaerobic bacteria:
- In oral healthy subjects, they are normally localized on the tongue dorsum in a large and extensive biofilm, as well as in the saliva [2].
- The percentage of these bacteria in the oral cavity is strictly linked with the patient’s habits, such as a diet rich in meat or smoking [3,4].
- the latest works report them as etiological agents in systemic infective-inflammatory or in autoimmune diseases such as rheumatoid arthritis and in atheromatous plaques [5-7], infective endocarditis and some researchers have recently suggested their role in neurogenerative diseases such as Alzheimer’s disease [8], while it is certain that F. nucleatum is associated with intestinal cancer.
This data suggests that the anaerobic bacteria resident in tongue microbiota play a direct-indirect role in modernday diseases due to our different habits as compared to our ancestors. In fact, recent works comparing the teeth microbiota in hundred-year old samples and present-day ones have demonstrated a substantial difference for these bacteria, especially in the Sonkransky red complex, where the modernday subjects exhibited a 100-fold increase in the percentage of red complex bacteria titer in the tooth calculus as compared to the old samples [9]. For such reasons, the increase in oral anaerobic bacteria in modern-day subjects, probably caused by different habits such as modern diet, can implement the risk for modern degenerative diseases.
Oral surgery and risk for bacteremia
The incidence of bacteremia and related systemic diseases due to oral anaerobic bacteria following different procedures such as: endodontic treatment, tooth extraction, periodontal surgery, tongue scraping and root scaling has been well documented [10-27] and anaerobe periodontal bacteria are isolated more frequently than facultative anaerobic bacteria, such as Streptococcus spp. [28]. Transitory bacteremia is detectable from 100 to 50% in healthy subjects after surgical acts, for example: dental extraction, tonsillectomy or third-molar surgery respectively. Surgical procedure could substantially increase the risk for oral bacteria systemic dissemination for three different reasons:
- mechanical breaking-down of the mucosa barriers for microorganisms, i.e. surface epithelium, immunological barrier of antibody-forming cells and defensins,
- non- effective use of antimicrobial agents during the surgical therapy [29],
- Immunosuppressed patient and
- Absence of a laboratory diagnosis to indicate oral salivary microbial status prior to the surgical act [30] (Figure 1).

Conclusion
Current evidence suggests that different systemic autoimmune or cardiovascular diseases, as well as oral -intestinal cancer, are related to different oral bacteria. In particular, recent years have seen the emergence of various anaerobic bacteria structured as biofilm in dental plaque and in tongue microbiota. These bacteria and their products may enter the bloodstream, thereby causing many systemic diseases and, sometimes, they are related to degenerative, autoimmune syndromes. Surgical procedures could interfere with the normal protective mucosa barrier and expose the patient to opportunistic oral bacteria. An effective control of systemic infections in oral surgery practice requires an operative protocol aimed at achieving specific objectives in: the pre-surgical step, during surgical procedure, and in the post-surgical step, including microbiological analysis, an accurate antimicrobial prophylaxis and a correct surgical procedure to avoid minimal lesions or traumas in the oral tissues.

Comments
Post a Comment