Juniper Publishers| Follicular Variant of Papillary Carcinoma Thyroid with Submandibular Lymph Node Metastasis
Journal of Surgery- JuniperPublishers
Abstract
Follicular variant of papillary carcinoma of thyroid (FVPTC) constitutes approximately 10% of papillary carcinoma of thyroid. Classic papillary carcinoma of thyroid (PTC) and the follicular variant of PTC have similar prognostic implications. The encapsulated follicular variant of PTC is usually quite indolent with an excellent prognosis. We report herein a case of a right follicular variant of papillary carcinoma thyroid with right submandibular lymph node metastasis. The diagnosis of follicular variant of papillary carcinoma of thyroid was made after histopathological examination of specimen after surgery.
Introduction
Follicular variant of papillary carcinoma of thyroid (FVPTC) whether invasive or not, behaves like usual PTC, with multiple tumor foci in the gland in many cases, lymphatic invasion and nodal metastases, and rare hematogenous spread [1,2]. FVPTC is defined by the presence of tumor cells arranged almost entirely in a follicular pattern with the nuclear features identical to that of PTC [3]. The median age of FVPTC is 44 years, similar to that of PTC which is 43 years [4]. The female to male ratio is 6:1 [5]. In the present study, we report a case of right follicular variant of PTC with right submandibular lymph node metastasis.
Case Report
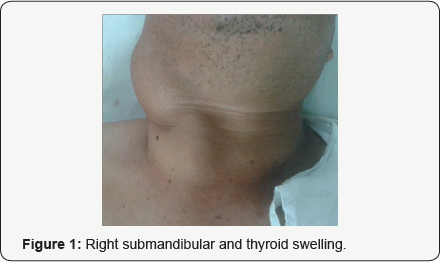
A 51 year old male presented with chief complain of swelling in right anterior neck for 6 years, swelling in right submandibular region for 6 years and dysphagia for 2 months. Patient complained of swelling in right submandibular region for 6 years which was insidious in onset, painless, progressive & increased in size for the last 2 months. He also complained of right anterior neck swelling for 6 years, which was insidious in onset progressive and painless. He complained of difficulty in swallowing for solids since 2 months. No h/o of difficulty in respiration, change of voice, bony pains or jaundice was reported. Patient was clinically euthyroid. Physical examination revealed A 8x5 cm2 swelling in right submandibular region which was hard, non-mobile, smooth with regular margin and another swelling 4 x 5 cm in size in right anterior neck that was hard, mobile , smooth surface with irregular margins and moves with deglutition (Figure 1).
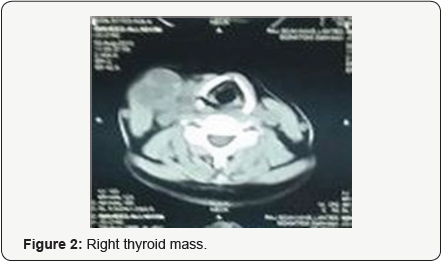
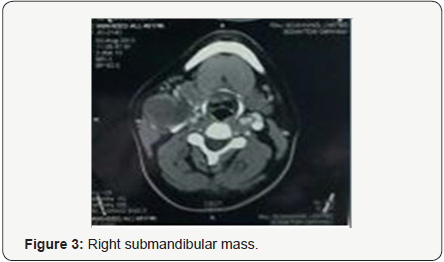
Blood investigations including thyroid profile were within normal range. FNAC was done from both the swellings and it was reported as follicular neoplasm. CECT neck showed ill-defined lesion with calcification (5.1 x 4.0 x 3.6 cms in size) is seen in right lobe of thyroid (Figure 2). Medially the lesion was abutting thyroid cartilage without osseous erosion. Lesion was having ill-defined interface with adjacent strap muscle and causing left lateral displacement of trachea. Posteriorly the lesion is abutting vertebral body of corresponding cervical vertebra w/o osseous erosion. Laterally the lesion is seen abutting carotid vessels and internal jugular vein with slight postero - lateral displacement. Another morphologically similar soft tissue lesion with necrotic areas and calcification (5.4 x 5 x 5.1 cms in size) is seen lateral to lesion described in right lobe of thyroid (Figure 3). No retrosternal extension of right thyroid lesion was present.
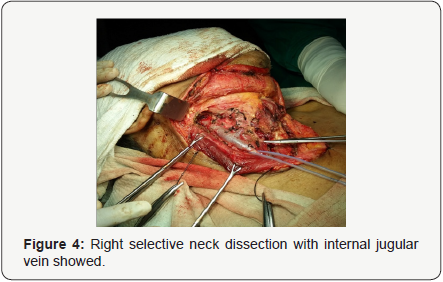
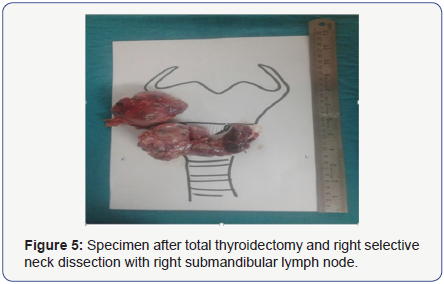
Indirect laryngoscopy showed bilaterally mobile vocal cords. Patient was optimized for surgery and total thyroidectomy with right selective neck dissection (supraomohyoid level I, II and III lymph nodes) was done (Figures 4 & 5). Both right and left recurrent laryngeal nerves were preserved. 3 parathyroid glands were identified and were preserved.Intraoperative and immediate postoperative period was uneventful with post op T - sign monitoring and serial total calcium & phosphorus remained within normal range. No immediate or late postoperative complications were noted. Stitch line was healthy & patient was discharged in satisfactory condition on 4th post operative day. Final Histopathology report came out to be follicular variant of papillary carcinoma thyroid with lymph node invasion. Patient was enrolled for postoperative radioactive iodine therapy. He is now asymptomatic with completely normal biochemical profile.
Discussion
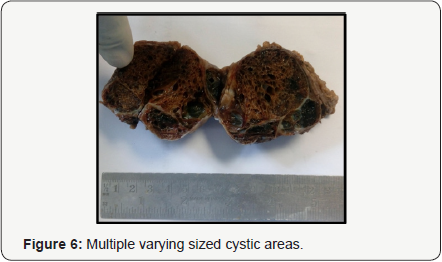
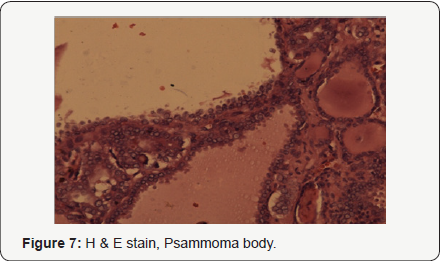
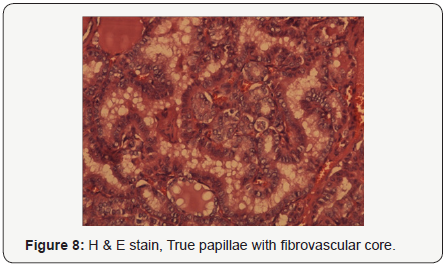
FVPTC constitutes approximately 10% of papillary carcinoma of thyroid. Classic papillary carcinoma of thyroid (PTC) and the FVPTC have similar prognostic implications. The encapsulated FVPTCis usually quite indolent with an excellent prognosis [1]. FVPTC, whether invasive or not, behaves like usual PTC, with multiple tumor foci in the gland in many cases, lymphatic invasion and nodal metastases, and rare hematogenous spread [2]. FVPTCis defined by the presence of tumor cells arranged almost entirely in a follicular pattern with the nuclear features identical to that of PTC [3]. The median age of FVPTC is 44 years, similar to that of PTC which is 43 years [4]. At the time of diagnosis, the rates of extensive extra thyroidal local spread, bilateral lesions, and vascular invasion were higher in FVPTC than those in PTC [5]. However, the risk for regional lymph node metastasis is lower than the classic PTC (Figures 6-8).
Conclusion
Although typically arising within the thyroid gland, occurrence in other organ sites has been reported, including the ovaries in struma ovarii and lingual thyroid [6,7]. Ultrasound imaging and fine needle aspiration have shown very low sensitivity for the diagnosis of FVPTC, making histologic examination the mainstay of diagnosis. As its name implies, FVPTC is defined histologically by the presence of follicular architecture throughout the tumor. The cellular features of FVPTC are identical to that of PTC and include clear nuclei, nuclear grooves, and pseudonuclear inclusions [8]. Psammoma bodies and a desmoplastic response at site of invasion are also frequent findings. FVPTC tend to have fewer calcifications and less psammoma body formation when compared to conventional PTC [9]. Management for FVPTC is same as that for PTC that is total thyroidectomy with therapeutic neck dissection of involved compartments for clinically apparent/biopsy proven disease with postoperative radioactive iodine ablation in selected cases.

Comments
Post a Comment