Juniper Publishers|Appendicectomies at a tertiary hospital: disease profile and surgical practices at Grey’s Hospital, Pietermaritzburg
Journal of Surgery- JuniperPublishers
Introduction
Appendicitis is one of the commonest causes of abdominal pain in both genders, occurring more often younger people [1], with the gender predominance varying across regions [1,2]. The causes of this disease are not clear, with several pathophysiological hypotheses having been proposed. The dietary fiber hypothesis suggests that the disease may be caused by the consumption of a low fiber diet. The hygiene theory suggests that improvements in water supply and sewerage disposal lead to an increase in appendicitis cases in Britain in the late 19th century by reducing children’s exposure to enteric organisms, leading to an altered immune response to viral infections [1,3,4].
The presentation of a temporal progression of acute central abdominal pain shifting to the right lower quadrant, associated with vomiting, subsequent mild fever and signs of peritoneal irritation, is diagnostic of appendicitis [3]. Laboratory inflammation makers complement the diagnostic tools, with reliance on clinical indicators alone resulting in a negative appendicectomy rate of 15% or higher, especially in women. The differential diagnosis includes various non-surgical and gynecological conditions, requiring careful consideration, with delay in diagnosis results in increased morbidity, such as perforation, and mortality.
In an attempt to improve diagnostic accuracy, the Alvarado scoring system, which uses six clinical and two laboratory features, was developed. A score of 0 to 4, 5 to 6, 7 to 8, and 9 to 10 suggests that the diagnosis of appendicitis is unlikely, possible, probable and definite, respectively [5]. Ultrasound and Computed Tomography (CT) scanning play a key role in reducing the higher rate of negative appendicectomy. CT scan is the most sensitive and accurate diagnostic method, but its specificity is similar to that of the ultrasound [6]. In cases of diagnostic uncertainty with a low suspicion index of appendicitis, conservative management, which includes hospitalisation and active clinical and laboratory observation, is an acceptable approach [3,7].
Kong et al. [8,9] validated the Alvarado score and in separate study, they evaluated the cost of managing appendicitis cases in Eden dale Hospital, a regional public sector hospital in Pietermaritzburg, South Africa. However, the profile of appendicitis patients, and the surgical procedures they underwent in Grey’s Hospital have not been fully studied. Current trends support an increased use of minimally invasive surgery for both diagnostic and therapeutic purposes, especially for women. The patients’ profile and clinical features influence the surgical management practices and the outcome. The surgical approaches utilized in Grey’s Hospital are also largely unknown. This information will help in improving patients’ care and benchmarking the institution against best practices and current trends; hence the relevance of undertaking this study.
Objectives
The study aimed to determine the demographic and clinical profile of patients treated for appendicitis, the commonest surgical approaches used for appendicectomy, the prevalence of post-operative complications, the prevalence of inaccurate diagnosis as demonstrated by the rate of histologically normal appendices, and the association between perforated appendix and, the age and gender of patients presenting with diagnosed acute appendicitis in Grey’s Hospital.
Methods
In a retrospective cross-sectional survey, we reviewed medical records of 196 patients who were operated for appendicitis between January 2011 and June 2012 in Grey’s Hospital, a tertiary hospital situated in Pietermaritzburg, South Africa. Theatre and laboratory registers were also reviewed to ensure completeness and accuracy of data. Variables collected included demographic data, surgical access, surgical procedure performed, complications, histology results and admission to intensive care unit (ICU). In this hospital, the diagnosis of appendicitis made by junior doctors is confirmed by a more experienced doctor before the patients are subjected to surgery.
Appendicectomy is carried out by a surgeon, registrar or an experienced Medical Officer, while postoperative management and follow up is done according to predetermined clinical guidelines, individualized according to each patient’s clinical presentation. Data was collected using a structured data collection sheet and analyzed using IBM-SPSS version 21 software. Frequency tables, Chi-square test of independence and logistic regression were computed to determine the prevalence of certain characteristics and establish association between the variables. Ethical approval for the study, and permission to use hospital records were obtained from relevant bodies of Pietermaritzburg Hospitals Complex. The imperative to obtain informed consent from individual patients was waved as this was a retrospective medical records review. At the time of data collection, all patients were either discharged or had died.
Results
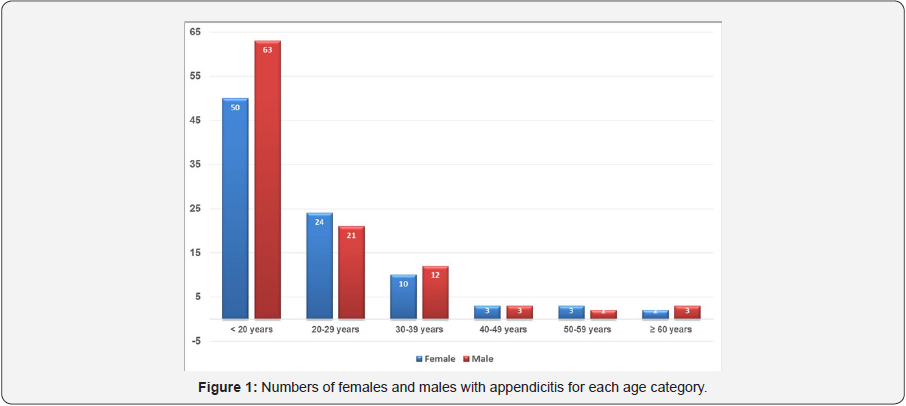
Hundred and ninety six patients’ records were reviewed, of which 53.1% were for male patients. The mean age of participants was 21.1 years (SD: 12.6), the range was 2-67years, and the majority (57.7%) of patients were <20 years. (Figure 1) shows that the gender distribution varied among the age groups, with more males in the younger age group (<20 years) but more females in the age group 20-29 years.
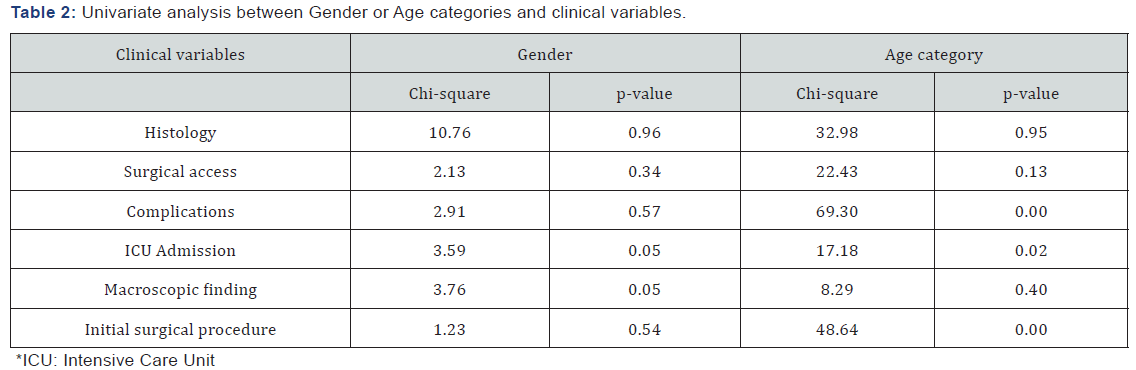
With respect to the prevalence of the clinical variables, the majority of patients had histology results that confirmed the diagnosis of acute appendicitis. The commonest surgical approach was the lower midline incision. Although most patients were discharged alive, one died, 19 were admitted to ICU, and three required bowel resection. Of the 15 patients who had a normal appendix on their histology report, 11 (73.3%) were females. Other clinical characteristics of the participants are presented in (Table 1). A univariate analysis of dependency showed no statistically significant association between ‘gender’ and all clinical variables. However, there were statistically significant associations 2, 10, 12-10-13, 2, 8, 9 between ‘age category’ and ‘complications’, ‘ICU admission’ and ‘initial surgical procedure performed’ (Table 2).
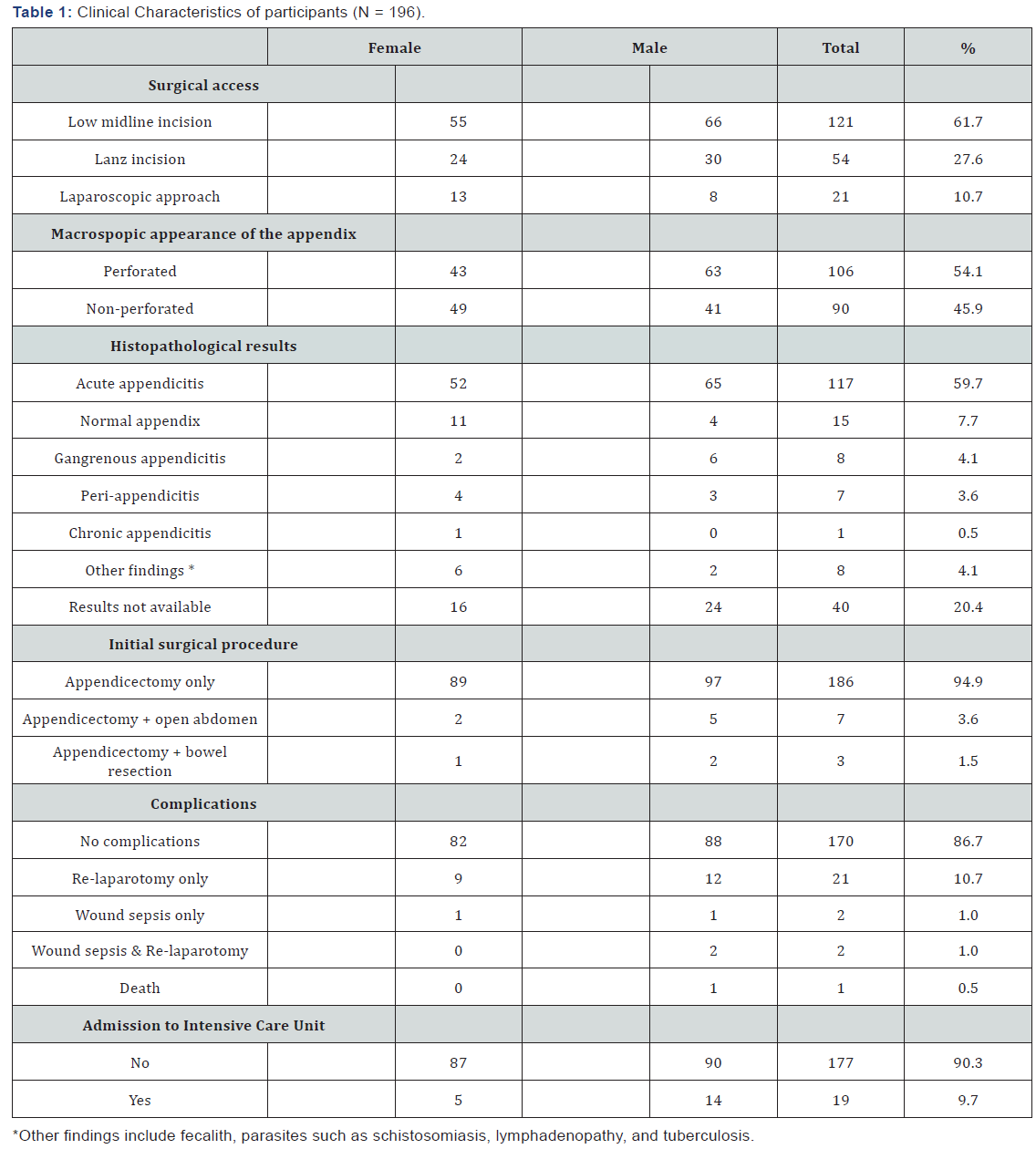
*ICU: Intensive Care Unit
A logistic regression performed to ascertain the effects of age and gender on the likelihood of a participant having a perforated appendicitis showed no statistical significance, χ2 (2) = 11.7, p = 0.16. The model explained only 2.5% (Nagelkerke R2) of the variance in perforated appendicitis and correctly classified 57.1% of cases. Males were 0.57 times (meaning a protective factor) more likely to have perforated appendicitis than females (p = 0.054, marginally not significant). Increasing age was not associated with an increased likelihood of perforated appendicitis (Table 3).
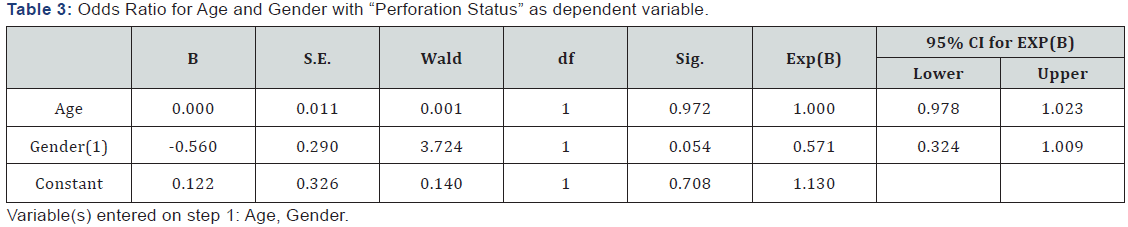
Variable(s) entered on step 1: Age, Gender.
Discussion
The mean age of our study participants was similar to that observed in other South African studies [2,8,9]. The predominance of males in the sample, although in keeping with findings in other studies [2,10-13], was not statistically significant (p = 0.054). Patients who were <20 years old accounted for 57.7% of the sample, which suggests that appendicitis is more common in younger patients [2,10,12-14]. The high number of younger patients presents a multiple challenges to the clinicians, as children are believed to have thin-walled appendices that are predisposed to perforation, leading to increased morbidity and/ or mortality. Children are also unable to give a reliable history and to cooperate fully during physical examination [15,16]. They commonly suffer from other comorbidities, such as upper respiratory infection, otitis media or gastroenteritis, making their clinical picture complicated, leading to a delay in diagnosis.
Similar to children under three years, appendicitis is the cause of severe morbidity and mortality in elderly patients [17,18]. The perforation rate in this study was 54.1% which is in keeping with the findings of Roger et al. [19] in the Eastern Cape. In contrast, 9.7% of our patients required ICU admission postsurgery versus 6.1% of patients in Prince Mshiyeni Memorial Hospital in Durban [12]. The preference of the midline incision in 61.7% of cases is well justified in the light of the high rate of perforated appendicitis (54.1%). Laparoscopic appendicectomy was used selectively in non-perforated appendices and in cases of diagnostic dilemma, as suggested by Ogbonna et al. [20]. The commonest incisions in Prince Mshiyeni Memorial Hospital were: lower midline laparotomy (47.2%), gridiron incision (37.3%), the combination of lower midline and gridiron incisions (5.6%), and laparoscopic surgery or long midline or Lanz incision (5.5%) [12]. These results may suggest a high rate of delayed presentation and/or complicated appendicitis. While these figures are in keeping with those found in this study, a study in the United Kingdom revealed a very low rate of open laparotomy of 10% [21].
The histological finding of normal appendix was more common in women; therefore the liberal use of imaging techniques, particularly ultrasound, and laparoscopic exploration should be encouraged in women. In a randomized study, Larsson et al. [22] showed that a negative appendicectomy rate of 34% with open appendicectomy could be reduced to 7% through the prior use of laparoscopy. In those patients who did not have appendicitis, a definitive gynaecologic diagnosis was made in 73% compared with only 17% who had open appendicectomy alone [22]. A study by Blisard et al. [23] showed that after implementing a clinical guideline recommending laparoscopic use prior to open laparotomy, a significant drop, from 31% to 23%, in the rate of negative appendicectomy in women was noted. Increasingly, laparotomy is being replaced by laparoscopic diagnosis and surgery [24].
Laparoscopy allows the appendix to be found wherever it may lie. The technique of laparoscopic appendicectomy is similar to the open operation, enabling the appendix to be visualized and an appendicectomy performed if it is abnormal. While a laparoscopic appendicectomy gives a lower wound infection rate and may allow an earlier return to normal activities, it is a more technically demanding operation [24]. In the absence of perforation and laparoscopic equipment, a low skin [12] and 2, 12, 13 crease incision (Lanz incision) rather than the higher and more oblique one centered on McBurney’s point is now favored as it gives a better cosmetic result.
Nonetheless, the advantages of laparoscopic versus open appendicectomy are not yet universally accepted. A Cochrane systematic review found that laparoscopic appendicectomy in adults, when compared to open surgery reduces wound infections, postoperative pain, length of hospital stay, and time taken to return to work. In the same review, the number of intraabdominal abscesses was higher after the laparoscopic surgery [25]. A recent review, however, found no significant differences between the two procedures, except higher quality of life scores at two weeks in the laparoscopic group. Kiriakopoulos et al. [26] reviewed post-operative complications on complicated appendicitis that were operated laparoscopically and found no wound sepsis or intra-abdominal abscesses. As the conversion to open surgery rate was only 4.8%, [27] the investigators recommended a laparoscopic approach even for complicated appendicitis.
At surgery, three types of appendicitis may be described: normal, simple acute and complicated (perforated and/or gangrenous appendicitis and/or peri-appendicular abscess) [24]. Of the 196 specimens submitted for histopathology, 7.7% were normal, 59.7% showed features of acute appendicitis, 4.1% were gangrenous and 3.6% showed signs of peri-appendicitis. Notwithstanding the fact that there were no histological results for 20.4% of cases, the rate of negative appendicectomy (7.7%) was similar to findings of other studies conducted in Africa [2,12,13]. Of the 15 patients who had normal appendix, 11 (73.3%) were females. This highlights the need for pre-surgical laparoscopic diagnosis in women to exclude gynecological causes of localized or generalized abdominal pains. A Nigerian study found that incorrect diagnoses were more commonly encountered in females [11].
The majority of patients (94.9%) had appendicectomy only, while 3.6% and 1.5% of patients had appendicectomy with the abdomen left open and with bowel resection respectively. These figures indicate that in most cases, the inflammation was limited to the appendix, suggesting that most of these cases could have benefited from laparoscopic surgery. Surgeons’ preferences and/or lack of skills may have been a limitation to choosing laparoscopic surgery. Post-operative complications were observed in 26 patients (13.7%), with 21 (10.7%) necessitating a re-laparatomy, four (2%) having wound sepsis, of whom two (1%) required a re-laparotomy, and one (0.5%) dying. Death accounted for 1.2% in Prince Mshiyeni Memorial Hospital [12]. The rate of post-operative infections in this study (2%) was significantly lower than those obtained in a Durban hospital (25.3%) in a Kenyan rural hospital (22%) [28].
Although the Chi-square test of association did not reveal any statistically significant association between ‘gender’ and all clinical variables, there was an almost statistical significance between it and ICU admission” and “macroscopic findings”. A statistically significant association between ‘age categories’ and ‘complications’, “ICU admission” and “the initial procedure performed” supports the finding of increased morbidity in extreme ages. Our model predicting the perforation status on the basis of gender and age revealed that being male was a marginally protective factor (OR = 0.57; p = 0.05; 95% CI = 0.324 - 1.009). It is not clear if infections from the gynaecologic tract played a role in this regard.
Limitations of the study
As with all retrospective charts review, some medical records had incomplete data which may have affected the findings. For example, the histology results were not available for 20.4% of cases. The study did not include cases that were taken to theatre for gynaecologic diagnosis that turned out to be appendicitis, as such patients might have had a pfannenstiel incision.
Conclusion
The majority of the patients reviewed present late with perforated appendicitis, resulting in midline laparotomy being the preferred surgical access despite the associated risk of additional morbidity. There is a need to develop skills in and encourage surgeons at this tertiary institution to perform minimally invasive surgery in cases of suspected appendicitis. The study has reaffirmed the difficulties in making the correct diagnosis in women, with 73.3% of patients with normal appendix being females. Judicious use of laparoscopy as an investigative and therapeutic tool may reduce the rate of negative laparotomy in women in particular.

Comments
Post a Comment