Saline-Filled Cuff-Punctured Percutaneous Dilatational Tracheostomy
Journal of Surgery- JuniperPublishers
Percutaneous dilatational tracheostomy (PDT) under
bronchoscopy and ultrasonography is safe and effective. Although cuff
puncture is a known adverse event during PDT, a saline-filled
endotracheal tube cuff might enhance ultrasound images and act as a
target for endotracheal puncture. Using a novel technique, the
saline-filled cuff can be identified and adjusted to the puncture
location under ultrasound. Once saline is withdrawn through the puncture
needle, the endotracheal tube is placed distally for detachment; the
needle tip remains in the trachea for guidewire insertion. Use of
dye-mixed saline, a tube exchanger during cuff puncture, and distal tube
placement enables effective PDT.
Keywords: Saline-filled cuff; Percutaneous Dilatational Tracheostomy; PDTIntroduction
Percutaneous dilatational tracheostomy (PDT) is
commonly performed in the intensive care unit. Numerous studies have
demonstrated the safety and effectiveness of PDT under bronchoscopy and
ultrasonography guidance [1,2]. However, a shortage of facilities and
specialists required for bronchoscopy and the need for technically
demanding ultrasound skills to identify both airway anatomy and position
of the endotracheal tube (ETT) may hinder the use of PDT [3]. Although
cuff puncture is generally recognized as an adverse event during the
procedure, a saline-filled ETT cuff may enhance the ultrasound images
and act as an ideal target for endotracheal puncture. We present our
initial experience and serial modifications of this novel technique.
Technique
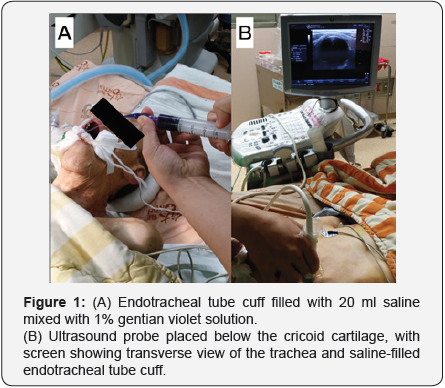
In the modified technique, the operator fills the ETT
cuff with 20 ml of colored saline mixed with 0.5 ml 1% gentian violet
solution for better visualization of the trachea using an ultrasound
linear probe placed below the level of the cricoid cartilage in
transverse scan, and gently adjusts the ETT cuff within the view of the
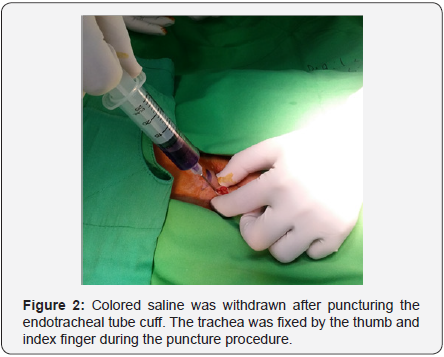
ultrasound probe (Figure 1). A small vertical incision is made in the
middle of the trachea at the level where the ultrasound probe been
placed. An introducer needle is used for puncture through the incision
with the trachea kept in place by the thumb and index finger (Figure 2).
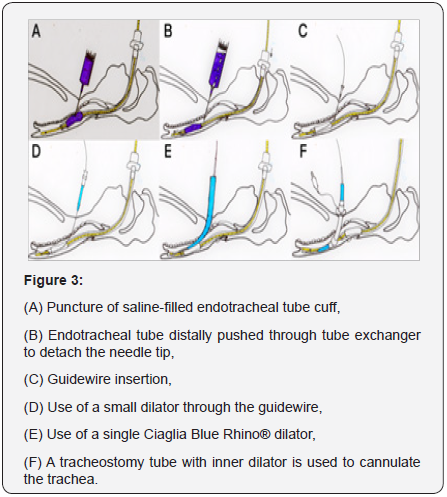
As the needle
is advanced into the ETT cuff, colored saline is withdrawn(Figure 3A).
When more than half of the colored saline has been withdrawn, the ETT is
advanced distally through the ETT exchanger and is detached from the
needle while the needle tip is still in the tracheal lumen, as confirmed
via air aspiration with a saline-containing syringe (Figure 3B). The
guidewire is then inserted through the introducer needle (Figure 3C) and
a standard PDT can be performed (Figure 3D-F). The video demonstrate
the entire procedure.
Comment
A saline-filled ETT cuff has been used to confirm adequate
placement of the ETT. A cadaver study [4] demonstrated that a
saline-filled ETT cuff allowed novice sonographers to accurately
visualize the ETT within the trachea, and a tracheal rapid
ultrasound saline test has also been used to confirm correct ETT
insertion depth in children [5]. In our institute, use of a salinefilled
ETT cuff improved sonographic visualization of the airway
anatomy and also helped to identify an adequate puncture
location for percutaneous dilatational tracheostomy (PDT).
However, repeated episodes of cuff puncture occurred during
our initial use of PDT; we found that the superior ultrasound
visualization provided by use of a saline-filled cuff was usually
accompanied by unintentional cuff puncture.
Recent clinical reports described ultrasound imaging of a
saline-filled cuff for accurate repositioning of the ETT during
PDT; however, only a description of the images and no details
related to the procedure had been reported [6]. Since the salinefilled
cuff appeared as an ideal puncture target on sonography,
we started our own cuff puncture PDT program using a larger
amount of saline (20 ml), which is safe for an ETT size 7.0 to 8.0
cuff, to enlarge the puncture target. After several initial cases, we
found that if saline was mixed with blood or airway secretions,
or if the amount of withdrawn saline was insufficient, we were
less confident in our ability to determine whether the needle tip
had punctured the ETT cuff; therefore, we used dye-mixed saline
for subsequent cases, and were able to satisfactorily confirm
accurate cuff puncture.
Real-time ultrasound-guided puncture is feasible for PDT,
but is not necessary if the puncture level has been previously
determined by ultrasound; moreover, it is helpful to fix the
trachea with index finger and thumb during cuff puncture. After
more than 30 cases, we identified a potential problem when
distal ETT advancement is not accurately performed, which
may result in the needle remaining in the cuff, with subsequent
failure of the procedure. This may be due to kinking of the ETT
in the oral cavity; therefore, we started to use a tube exchanger
for effective inward placement of the ETT, which has worked
well. A recent clinical study also described inward placement
of the ETT during PDT without outward placement of the tube
[7], thus lowering the risk of inadvertent ETT dislodgement.
By using dye-mixed saline and a tube exchanger during cuff
puncture, and distal placement of the ETT, the procedure can be
performed more effectively and with confidence, and provides
an alternative technique for PDT.

Comments
Post a Comment