JuniperPublishers-Anatomical Variation of the Anterior Cutaneous Branch of Femoral Nerve: A Case Report
Journal of Surgery- JuniperPublishers
Abstract
The femoral nerve is the largest branch of lumbar plexus. It arises from the dorsal branches of the second to fourth ventral rami. By passing behind the inguinal ligament into the thigh, it is split into the anterior and posterior divisions by the lateral circumflex femoral artery. The branches from the anterior divisions are mainly to the sartorius muscle and two cutaneous branches, that is, the medial and intermediate cutaneous branches of thigh. This article reports a case of anatomical variation of the anterior cutaneous branch of femoral nerve. The anterior cutaneous branch of femoral nerve after dividing into two terminal branches, the medial cutaneous nerve pierces the sartorius muscle. We have to be aware of these types of nerves when an operation is performed around this area, and the patient should be informed about the chance of injury to the nerve as referred to in this article.
Keywords: Femoral nerve; Variation; Anterior cutaneous nerve
Introduction
The anterior cutaneous branch of femoral nerve (ACBFN) is one of the cutaneous nerves of thigh. This nerve consists of the following nerves; an intermediate cutaneous nerve and a medial cutaneous nerve. The intermediate cutaneous nerve (middle cutaneous nerve) pierces the fascia lata (and generally the Sartorius muscle) about 7.5 cm below the inguinal ligament and divides into two branches which immediately descend on the front of thigh to supply the skin as low as the front of knee. Here, they communicate with the anterior division of lateral cutaneous nerve, the anterior division of medial cutaneous nerve, and the infrapatellar branch of saphenous to form the patellar plexus. In the upper part of thigh, the lateral branch of intermediate cutaneous joint with the lumboinguinal branch of genitofemoral nerve. The medial cutaneous nerve (internal cutaneous nerve) passes obliquely across the upper part of femoral artery sheath and divides in forepart, or at the medial side of that vessel, into two branches, an anterior and a posterior.
The anterior branch runs downward on the sartorius, pierces the fascia lata at the lower third of thigh, and divides into two branches; one supplies the integument as low down as the medial side of knee and other crosses to the lateral side of patella, communicating in its course with the infrapatellar branch of saphenous nerve. The posterior branch descends along the medial border of the Sartorius muscle to the knee, where it perforates the fascia lata, communicates with the saphenous nerve, and gives off several cutaneous branches. It then passes down to supply the integument of the medial side of leg [1]. Due to rarity the course of this nerve, there aren’t any papers about variation of this nerve. In the present case, a rare variation of the anterior cutaneous branch of femoral nerve (medial cutaneous part) that pierces the sartorius muscle is presented.
Case Report
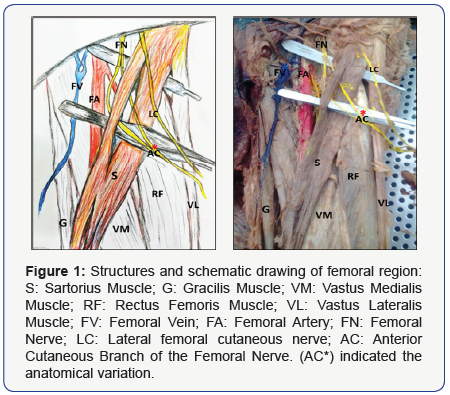
During anatomical dissection of the left lower limb of a male Iranian cadaver in the Medical Faculty of Tabriz University of Medical Sciences, an anatomical variation of the anterior cutaneous branch of femoral nerve course was recognized. The skin and fascia of left lower limb were completely dissected, and the neurovascular bundle of femoral region and the whole limb were clearly explored. The course of the nerves and their branches were thoroughly traced and the observed anatomical variation was recorded. The anterior cutaneous branch of femoral nerve after dividing into the intermediate and medial cutaneous nerves, the medial cutaneous nerve pierces the sartorius muscle and continues course itself (Figure 1). The other branches of femoral nerve had the normal anatomical course. Also, the vessels and the other nerves of femoral region hadn’t any anatomical variation.
Discussion and Conclusion
As per standard textbooks of anatomy, the femoral nerve is the largest branch of lumbar plexus and it arises from the posterior division of anterior (ventral) rami of the second, third, and fourth lumbar nerves. The femoral nerve descends on the psoas major muscle and enters the thigh deep to the inguinal ligament at the lateral edge of femoral sheath, which separates it from the femoral artery. Distally to the inguinal ligament, the femoral nerve divides into two branches; the anterior and posterior divisionsby the lateral circumflex femoral artery. The branches from the anterior divisions are mainly to the sartorius muscle and two cutaneous branches, that is, the medial cutaneous nerve of thigh and the intermediate cutaneous nerve of thigh [2].
Kennethshowed the major branches involved in standing (vastus medialis, vastus intermedius, and vastus lateralis nerves) centrally located, whereas the sensory branches and the branches not implicated in standing (saphenous, medial cutaneous, sartorius, and rectus femoris nerves) located in the medial or lateral part of branching pattern [3]. Aizawa reported that the medial cutaneous nerve branches and vastus medialis, vastus intermedius, Vastus lateralis, and rectus femoris nerves were arranged medially to laterally, respectively [4]. Gustafson reported this pattern except in two specimens where the sartorius nerve was located between two cutaneous branches [3]. Aizawa reported that the medial cutaneous nerve branch and the adductor longus branches were the first two branches to leave the femoral nerve in the thigh [4].
As paresthesias or pain observed in the anterior thigh, lateral thigh and gluteal regions might be due to compression of the ACBFN, surgeons must always remember the possible variations of the ACBFN during surgical procedures to prevent injury to it [5,6]. We propose that further research should be conducted to investigate the relationship between anatomical variation and its effect on patient presentation and differential diagnosis, most specifically with regard to the effect of anatomical variation on neural mechanosensitivity. Also, nerve morphology and fascicular anatomy information are of value for neurosurgical procedures, such as nerve anastomosis procedures for recovery of function after traumatic injury, similar to the hypoglossalfacial nerve anastomosis that is used to treat peripheral facial nerve paralysis [7].

Comments
Post a Comment