JuniperPublishers- Video Assisted Anal Fistula Treatment “VAAFT Technique” for Complex Perianal Fistulas
Journal of Surgery- JuniperPublishers
Abstract
A novel sphincter saving technique (video assisted anal fistula treatment or VAAFT) was used in a prospective randomized study to validate the efficacy of this technique in complex anal fistulas. Two groups of 12 patients were randomly selected to undergo this study and were followed for 24 months. One group was subjected to VAAFT and the other group to open fistulotomy. We had one recurrence and 2 failures in the VAAFT group leading to repeated procedures. There was no sphincter affection in the VAAFT group compared to 4 patients with transient incontinence in the open group. To conclude, video assisted anal fistula treatment (VAAFT) is a novel sphincter saving technique in the management of for complex anal fistula (PAF). Further studies on larger number of patients may be needed to establish the role of this approach in fistula treatment.
Abbreviations: VAAFT: Video Assisted Anal Fistula Treatment; IO: Internal Fistula Opening; MRI: Magnetic Resonance Imaging; LIFT: Ligation of the Intersphincteric Tract
Introduction
Current surgical techniques for treating anal fistulas are bases on three main principles: identification of the fistula tract(s) and the internal opening(s), excision of the fistula tract(s) and preservation of the anal sphincters. Fistulotomy/fistulectomy is the gold standard in the treatment of anal fistulas with only minor involvement of the anal sphincters [1]. Complex anal fistulas are very challenging for the surgeon because of the risk of sphincter affection after traditional surgical approaches. Complex anal fistulas according to Park’s, are identified as those fistulas in which cannot be adequately treated by simple fistulotomy [2]. The rationale of VAAFT based of the concept of both detection and perfect closure of the internal fistula opening (IO), in addition to the destruction of the tract and cleaning which will allow complete and definite healing [1]. The aim of this pilot study is to validate the efficacy of VAAFT procedure for curing complex anal fistulas compared to traditional fistulotomy (with or without seton).
Patients and technique
This study was conducted in our unit (unit 6) Department of general surgery; Ain Shams University in the period from December 2013 till December 2014 and patient s were followed for 24 months. Two groups of 12 patients with complex anal fistulas were subjected to a randomized study where the first group underwent open fistulotomy with or without seton) and the second group underwent VAAFT. The type of fistula was determined by the preoperative investigations including the following: physical examination, endo-anal ultrasound and MRI. Randomization was one to one by closed envelope technique. Exclusion criteria were simple low anal fistulas, recto-vaginal fistulas and refusal of the procedure. Informed consent was taken from all patients and the study was approved by our local Ethics committee.

The open fistulotomy was done in the usual fashion under spinal anesthesia and a seton was used optionally in case the whole tract could not be laid open for fear of sphincter affection especially if the fistula tract involved more than 1/3 of the sphincter complex. The VAAFT procedure, on the other hand, is performed using a kit (Figure 1) manufactured by Karl Stortz GmbH (Tuttlingen, Germany), which includes the fistuloscope, an obtuorator, a unipolar electrode, an edobruch and an endoforceps. The fistuloscope has an 8°angled eyepiece and is equipped with an optical channel and a working and an irrigation channel. Its diameter is 3.3 X 4.7 mm, and its working length is 18 cm. A removable handle allows easier manipulation of the scope. The fistuloscope has 2 taps, one which is connected to a 5000 ml bag of glycine-mannitol 1% for irrigation. The VAAFT procedure was carried on under spinal anesthesia with patient in lithotomy position. According to Meinero and Mori, the procedure consisted of two phases: a diagnostic phase and a therapeutic phase [1].

The diagnostic phase: The purpose of the diagnostic phase is to correctly locate the internal fistula opening and possible secondary tracts or abscess cavities. The fistuloscope was assembled and connected to the video monitor (Figure 2). The fistuloscope was inserted through the external opening with the glycine-manitol solution already running. In case the external opening was narrow or fibrosed we excised a small area of the external opening scar or skin surrounding it (Figure 3). The obturator was visible during insertion of the fistuloscope into the fistula tract at the lower edge of the screen to ensure the correct orientation of the fistuloscope. The fistula tract was apparent clearly on the screen (Figure 4).


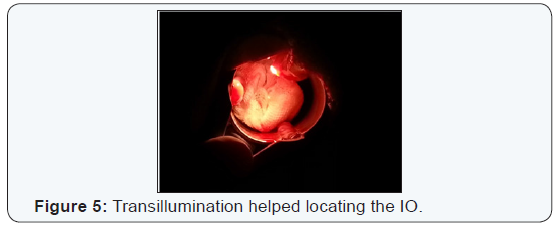
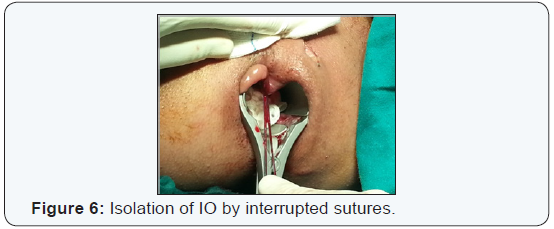
The fistuloscope was simply advanced along the pathway using slow movements, left to right and up/down, helped by the pressure gradient of the irrigation solution opening the tract as we advanced the scope. These manoevers allowed the fistulas to accommodate the fistuloscope in most of the cases and the fistulas were straightened. Spinal anesthesia facilitated this process. Optimal vision of the lumen of the fistula was ensured by jets of irrigation solution reaching to the internal opening (IO) of the fistula tracts. At that point the assistant inserted anal retractor and the lights in the operating theater were dimmed so that it was easy to see the fistuloscope in the rectum. The fistuloscope usually exited from the internal opening. Sometimes the IO was very narrow and the location of the orifice was only identified by observing the fistuloscope light behind the rectal mucosa (Figure 5). At this point we inserted 3 interrupted vicryl sutures around the IO in order to isolate it but not to close it for the time being (Figure 6).
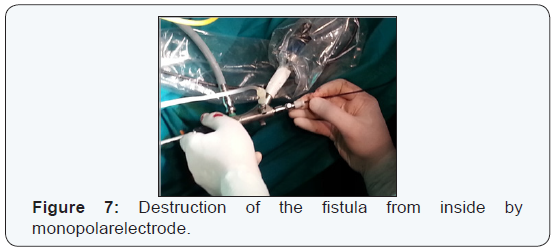
The operative phase: The goals in this phase was the destruction of the fistula tracts from within, cleansing of the fistula tracts and finally closure of the IO. First we removed the obtuorator and replaced it with the monopolar electrode, which fulgrated the fistula tracts under direct vision. We proceeded centimeter by centimeter from the external opening to the internal opening cauterizing all fragments of whitish material adherent to the fistula wall and taking care not to overlook any abscess or any possible fistula side tract. Continuing under direct vision, necrotic material was removed by the endo-brush or a Volkmann spoon (Figure 7).
The continuous jet of irrigation solution also ensured that all the waste material was eliminated into the rectum through the internal opening, which was left open and isolated by stitches but not yet closed. At this point the assistant exerted tension on the stitches so that the IO was lifted in the rectum like a volcano. A linear stapler was used to close the internal opening completing the mechanical air tight closure of the IO (Figure 8). The result was simply a linear staple line in on the mucosa of the rectum and a very small perineal scar which was left open to drain the fistula tract till complete healing. We used internal mucosal flap in some cases to close the internal opening in cased where the IO was tough and thick or when staplers were not available. We did not use synthetic cyanoacrylate to buttress the IO as in the description of Meinero due to several reasons, the least of which was unavailability and to reduce the cost and abscess formation.

Continence was followed up using telephone interview and was evaluated further in post-operative follow up visits by digital rectal examination with or without anorectalmanometry if needed. The questionnaire included 4 points each given a score of 0-3. The patients who did not have incontinence was rated 0, those with incontinence to flatus were given 1, those with incontinence to liquid stools or with mucous leak were given 2 and finally those with incontinence to formed stools were given a score of 3.
Results
We had 19 males and 5 females, all with complex anal fistulas. In the VAAFT group we had 10 trans-sphincteric fistulas, one horshoe fistula and one extrasphincteric fistula. In the fistulotomy group we had nine trans-sphincteric fistulas, 2 horseshoe fistulas and one supra-sphincteric fistula. We had 2 failed VAAF procedures, one due to a horseshoe fistula tract in which the scope could not reach the IO, and the other case was because of sclerosis of the tract. We had no failed filtulotomy cases. The two failed VAAFT cases were treated with LIFT in one case and fistulectomy with coring out of the tract in the other case. We did not needseton in fistulotomy group. The IO was located in 11 patients of the VAAFT group (92%) and in 10 of the fistulotomy group (83%). Operative criteria and postoperative complications of both groups are illustrated in (Table 1). Follow up for more than 6 months was 92% for both groups. The operative time was prolonged in the VAAFT group in the beginning of the series but the time was approaching that of fistulotomy group by the end of the study to about 35 minutes.
We had one postoperative recurrence in the VAAFT patients in comparison of 2 recurrences in the fistulotomy group.
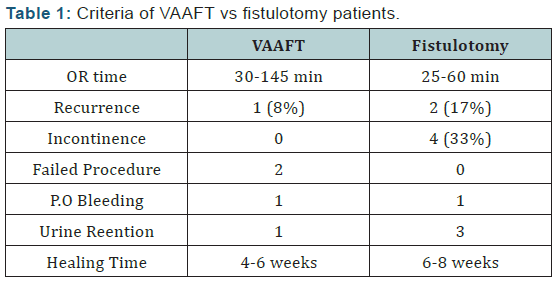
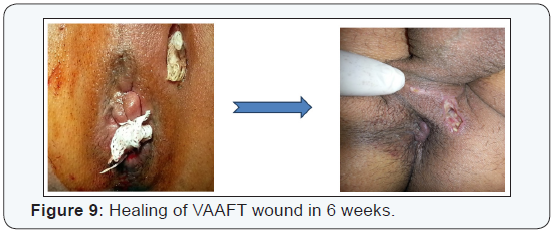
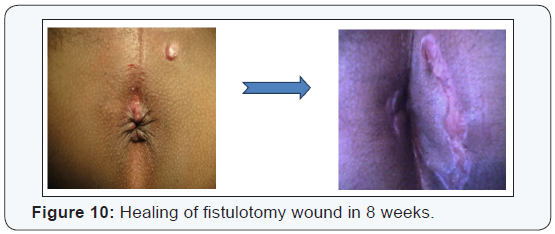
The patients in the VAAFT 4-6 weeks to complete healing whereas in the fistulotomy group it took 6-8 weeks in some patient especially with big perineal wounds (Figures 9 & 10). As regards continence, the patients in both groups were evaluated by questionnaire and clinical examination. There was no gross fecal incontinence in VAAFT (zero% incontinence) group but there were four patients with transient incontinence in the fistulectomy group (33%); two patients with incontinence to flatus (scored 1) for 2 weeks, with two other patients with incontinence to liquid stools (scored 2) with weak anal tone which returned spontaneously to normal after one month. The anal sphincter tone was clinically normal in all VAAFT patients postoperatively.
Discussion
The patient’s first visit and correct initial surgical treatment play a fundamental role in fistula treatment. The key for successful fistula treatment is identification of the internal opening (IO), excision of the tract and preservation of anal sphincter function. Fistulotomy/ fistulectomy are the gold standard in the treatment of anal fistulas with only minor involvement of the sphincters. Complex fistulas are challenging for the surgeon because of the high incidence of incontinence after traditional procedures. Philips et al reported 96% healing rate using lay open fistulotomy in management of complex fistulas but with 30% incidence of incontinence to flatus, 2% for soft stools and 4% for hard stools respectively [3].
That is why the VAAFT technique is based on a concept that avoids sphincter dysfunction (minimally invasive) as well as allowing detection of and perfect closure of the IO, in addition to destroying and cleaning the fistula pathway which will allow definite healing in a way [1]. The efficacy of other sphinctersaving procedures varies considerably, Fibrin glue is a technically easy low risk procedure but results were disappointing with failure rates up to 84% [4-8]. The same applies for Fistula Plug, a simple sphincter saving procedure but very expensive technique with variable success rates ranging between 29-87% [9-14]. Ligation of the intersphincteric tract (LIFT) consists of ligation of the fistula tract in the intersphincteric plane, and like VAAFT, is based on the principle of secure closure of the internal opening. It has success rates up to 95% [5,15-17]. However, ligation of the internal opening in the intersphincteric plane may be technically difficult especially in case of trans-sphinteric and horseshoe tracts, with the risk of sphinter damage or ischemia, leading to failure or incontinence [18].
Fistula laser closure (FiLaC™), like VAAFT, is based on the principle of closing the internal opening using a flap with laser obliteration of the fistula tract. The preliminary results obtained were 83% cure rate, but unlike VAAFT, this procedure is performed blindly without the advantage of visualizing the side tracts or abscesses [19]. As regards VAAFT, this procedure is based on the principle of adequate closure of the internal opening as well as obliteration of the fistula tract. The real innovation is the ability to visualize internal opening and identification of the fistula anatomy by fistuloscopy and of obliteration of the tract by fulguration under direct vision [1]. The other proposed advantages were the ability of identification of all side tracts and abscess cavities connected with the main tract. The air tight closure of the tract by stapler or sutures as proposed by Meinero and Mori together with reinforcement of the staple line from the inner side achieved 87% cure rate after 1 year follow up [1].
This study showed an overall success rate of 84% with a cure rate of 92% after 24 months follow up. On the other hand, failure of such procedure in 2 cases was attributed to the fact that some fistula tracts were hors-shoe, or totally sclerosed and fibrotic subsequently making progress of the scope impossible or dangerous.In such cases we adopt the fistulotomy technique with or without Seton according to the situation. On the other hand, the operative time was initially prolonged in the VAAFT group reaching up to 145 minutes, due to the learning curve, but by the end of the study the technique was mastered and our operative time was reduced to 30 minutes, comparable to Meinero and Mori [1]. This study also demonstrates the efficacy VAAFT in the management of complex PAF with IO located in 92% of cases with the lowest recurrence of 8%, compared to 17% in the fistulotomy group which could be distressing to patients and with minimal accepted complications.
Continence was objectively evaluated in this study, unlike the initial one published by Meinero in 2011, and it showed that VAAFT is a real novel sphincter saving technique with minimal or no effect on anal continence (zero incontinence) unlike fistulotomy which carries the risk of some degree of incontinence ranging from minor incontinence which was 33% in this study, to major fecal incontinence if not used judiciously. Fortunately, we had none. To conclude, video assisted anal fistula treatment (VAAFT) is a novel sphincter saving technique in the management of for complex anal fistula (PAF). Also VAAFT ensures adequate localization of IO and management of the fistula tract without affecting anal continence. However, VAAFT may not be suitable for adequate management of hors-shoe PAF. The results are promising, but future randomized controlled studies may be needed to draw a solid conclusion and establish the role of this technique in the management of anal fistulas.
To read more articles in Journal of Surgery
For More Open Access Journals in Juniper Publishers

Comments
Post a Comment